Ketamine has gained attention in recent years for its off-label use in treating depression, PTSD, and chronic pain. Once known primarily as a dissociative anesthetic used in operating rooms and veterinary clinics, ketamine is now being used in mental health clinics across the world. But like any drug, ketamine comes with risks—and understanding both the short-term and long-term side effects is essential before considering it for medical or recreational use.
What is Ketamine?
Ketamine is a dissociative anesthetic developed in the 1960s. It’s still used in hospitals for anesthesia and pain management. More recently, ketamine—especially its S-enantiomer version, esketamine—has been FDA-approved for treatment-resistant depression under the brand name Spravato.
Unlike many antidepressants, ketamine works quickly—often within hours—by targeting glutamate pathways in the brain. However, its potential for abuse, addiction, and long-term neurological impact makes it a drug that needs careful supervision.
Short-Term Side Effects of Ketamine
Ketamine’s short-term effects can range from mild to intense, depending on the dose, route of administration (oral, intranasal, intravenous, or intramuscular), and the individual’s physical and mental health status.
1. Dissociation and Hallucinations
One of the most prominent short-term effects of ketamine is dissociation. Users often describe an “out-of-body” experience or feeling detached from reality. This is sometimes called entering a “K-hole”—a deeply dissociative state marked by impaired sensory perception and distorted time and space awareness.
This can be distressing, especially for first-time users or those with underlying psychiatric conditions. In medical settings, it’s managed carefully, but recreational users may find the experience overwhelming or frightening.
2. Cognitive and Motor Impairment
Ketamine can impair memory, judgment, attention, and coordination shortly after use. This is why operating heavy machinery or driving under the influence of ketamine is extremely dangerous. It also slows reaction time and affects spatial reasoning.
3. Elevated Heart Rate and Blood Pressure
Ketamine causes a surge in sympathetic nervous system activity, which can lead to:
- Increased heart rate
- Elevated blood pressure
- Shortness of breath
- Nausea and vomiting
For individuals with cardiovascular problems, this effect can be dangerous.
4. Nausea and Vomiting
Post-infusion nausea is a common side effect in clinical settings. Some people experience dizziness or vomiting, particularly when ketamine is administered quickly or at high doses.
5. Anxiety or Agitation
Though ketamine is used to treat depression and anxiety, some users experience acute anxiety or panic during a trip. These reactions are often linked to set and setting—meaning the person’s mindset and the environment in which the drug is taken.
6. Slurred Speech and Drowsiness
As a central nervous system depressant, ketamine can make users feel sleepy, dazed, or mentally clouded. It may also cause slurred speech and impaired verbal communication during the acute phase.
7. Bladder and Urinary Problems (with frequent short-term use)
Frequent recreational users, even in the short term, may start to develop bladder pain or frequent urination—a sign of emerging urinary tract toxicity. This is rare in medical use but more common in chronic recreational users.
Long-Term Side Effects of Ketamine
The long-term effects of ketamine use are more concerning, especially with repeated, high-dose, or unsupervised use. Some of these effects may be reversible; others can lead to lasting damage.
1. Cognitive Impairment
Long-term ketamine use has been linked to:
- Memory deficits
- Reduced attention span
- Impaired executive function
- Slower processing speed
Some of these effects appear to reverse after stopping use, but prolonged or heavy use may lead to more permanent damage, particularly in younger users whose brains are still developing.
2. Bladder and Kidney Damage
One of the most serious long-term side effects of ketamine is ketamine-induced cystitis—a painful, chronic inflammation of the bladder. Symptoms include:
- Urinary frequency and urgency
- Painful urination
- Blood in urine
- Reduced bladder capacity
Left untreated, this condition can lead to permanent bladder damage and kidney problems. In some cases, surgery or bladder reconstruction may be necessary.
3. Psychological Dependence
While ketamine doesn’t cause classic physical withdrawal symptoms like opioids or alcohol, it can be psychologically addictive. Users may develop a strong craving for the dissociative or euphoric effects, leading to frequent use and difficulty stopping.
Some signs of ketamine dependence include:
- Using more than intended
- Failed attempts to quit
- Spending a lot of time obtaining or using ketamine
- Using ketamine to cope with stress or emotions
4. Depression and Mood Instability
Ironically, while ketamine can relieve depression in the short term, chronic recreational use has been linked to worsening mood, increased anxiety, and even suicidal thoughts over time. This may be due to neurochemical changes in the brain or the psychological fallout of dependency and withdrawal.
5. Liver Function Changes
Chronic ketamine use can affect liver enzymes and lead to impaired liver function in some users. Though this is more common with high doses or long-term use, regular monitoring is recommended for those using ketamine therapeutically over months or years.
6. Tolerances and Diminished Therapeutic Effect
Repeated ketamine use may lead to tolerance, meaning higher doses are needed to achieve the same effect. In clinical settings, this limits how often ketamine can be used effectively for depression or pain management. Some users also report a “blunting” of the antidepressant response over time.
7. Risk of Psychosis
In vulnerable individuals, especially those with a family history of schizophrenia or bipolar disorder, ketamine may trigger or worsen psychotic symptoms. Though this is rare in controlled environments, it’s a serious risk in unsupervised or frequent recreational use.
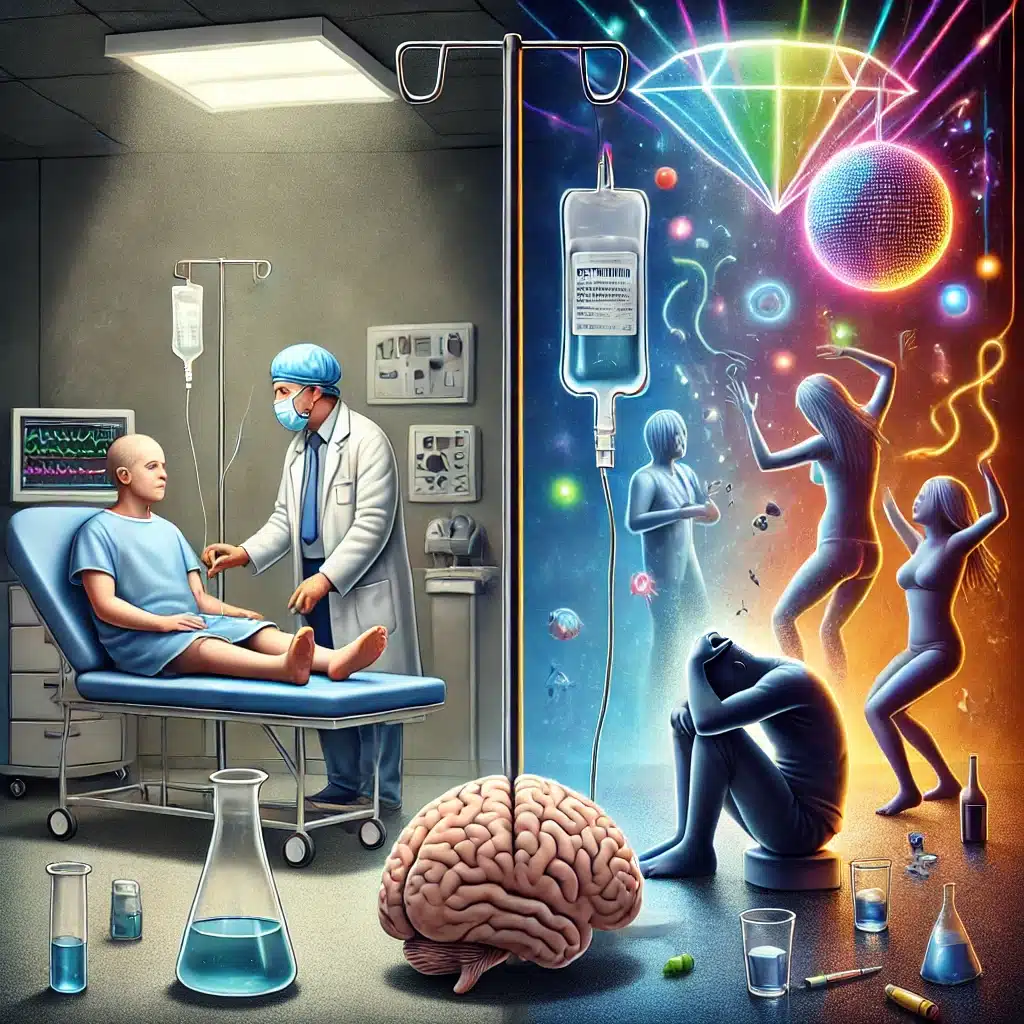
Medical vs. Recreational Use: A Key Difference
It’s important to distinguish between clinical use of ketamine and recreational abuse. When used under medical supervision:
- Doses are controlled
- Use is time-limited
- Patients are screened for risk factors
- Side effects are monitored and managed
Recreational use, by contrast, is unpredictable. Doses vary, routes of administration are riskier (e.g., snorting, injecting), and users may combine ketamine with other substances like alcohol, benzodiazepines, or stimulants—all of which increase the risk of harm.
Harm Reduction and Safety Tips
For those who choose to use ketamine recreationally or are undergoing clinical treatment, harm reduction is key:
- Stay hydrated: Especially to protect the bladder and kidneys.
- Don’t mix with other depressants: Combining with alcohol or benzos increases overdose risk.
- Use in a safe, quiet environment: To reduce the risk of panic or injury during dissociation.
- Limit frequency: Regular breaks can prevent tolerance and long-term damage.
- Monitor mental health: Watch for signs of dependency, depression, or mood swings.
If you’re considering ketamine therapy for depression or pain, work with a licensed medical provider experienced in ketamine treatment. Avoid DIY approaches or buying ketamine on the black market—purity, dosage, and safety can’t be guaranteed.
Final Thoughts
Ketamine is a powerful drug with real medical potential—but it also carries real risks. In the short term, it can cause dissociation, nausea, high blood pressure, and cognitive impairment. Long-term use raises concerns about bladder damage, cognitive decline, dependency, and mental health issues.
Used responsibly and under medical supervision, ketamine can be a breakthrough therapy. But used recklessly, it can become a source of serious harm. Like many substances, the line between medicine and poison depends on context, dose, and intent.
If you’re curious about ketamine treatment or concerned about your ketamine use, speak with a doctor, psychiatrist, or addiction specialist. There are safer paths forward—and support is available.