Approx. read time: 6.8 min.
Post: AI in Diabetes Treatment and Prevention
A New Era in Diabetes Care-AI in diabetes treatment and prevention
Diabetes has long been one of the world’s most burdensome chronic diseases, affecting over 500 million people globally. For decades, managing diabetes meant a rigid routine of finger pricks, insulin injections, and diet control—often guided by trial and error. But that’s changing fast.
Artificial intelligence (AI) and emerging technologies are rewriting the rules of diabetes care. From real-time glucose tracking to predictive algorithms that warn of future complications, today’s tools are smarter, faster, and more personalized than ever before. This isn’t just about convenience—it’s about saving lives and improving quality of life for millions.
This article explores how AI and digital technology are revolutionizing both the treatment and prevention of diabetes—and why this shift matters now more than ever.
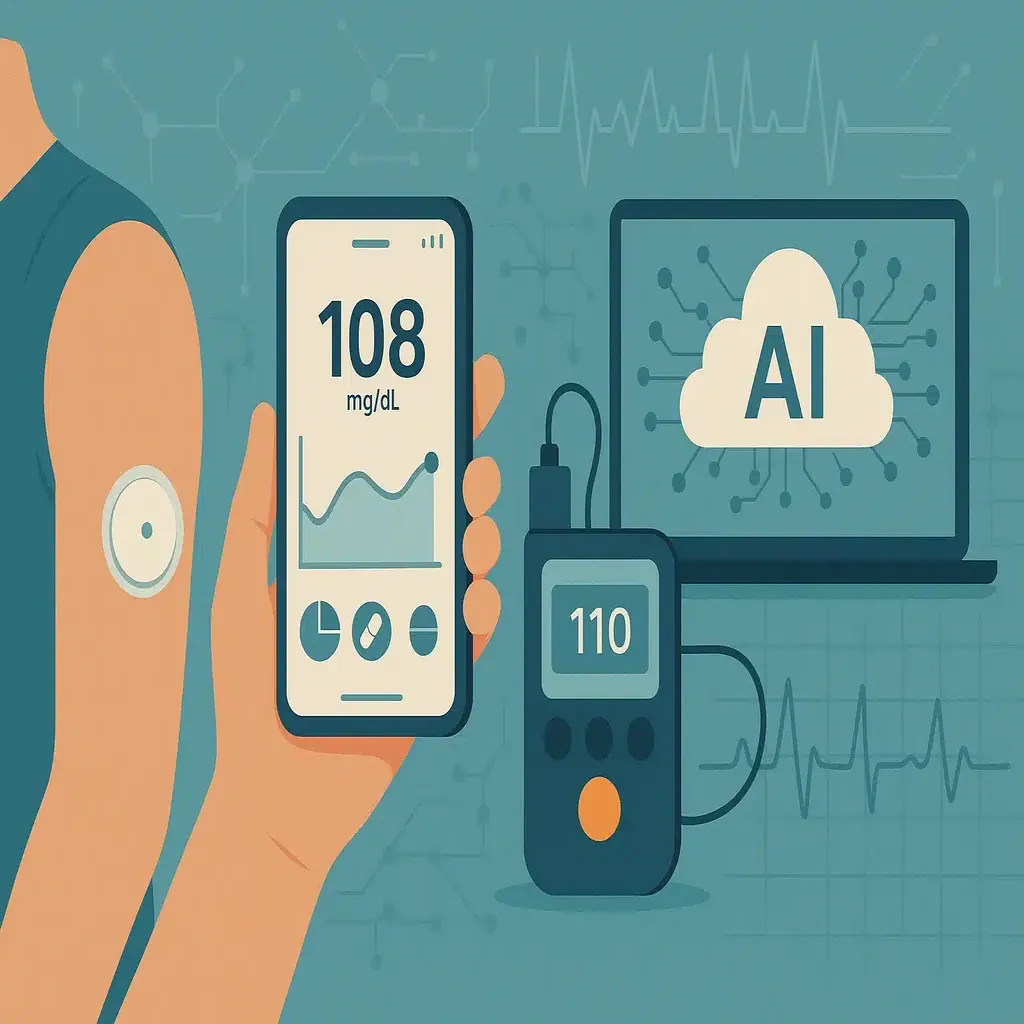
1. Real-Time Glucose Monitoring and Automated Insulin Delivery
Perhaps the most visible advancement in diabetes tech is the rise of continuous glucose monitoring (CGM) systems. Devices like the Dexcom G7 or Abbott’s FreeStyle Libre use small sensors inserted under the skin to track glucose levels 24/7. These sensors send data to smartphones or wearable devices, providing users with live updates and trend analysis.
But the real breakthrough comes when CGMs are paired with AI-driven insulin pumps, creating what’s known as a hybrid closed-loop system—or more informally, an “artificial pancreas.” Brands like Medtronic and Tandem have developed systems that adjust insulin delivery automatically based on CGM feedback. This means fewer manual interventions, fewer dangerous highs and lows, and tighter overall glucose control.
Impact: These smart systems reduce A1C levels, decrease hypoglycemia episodes, and give users more freedom and peace of mind.
2. Personalized Treatment Plans Powered by AI
Every person with diabetes is different. Variables like age, weight, activity level, meal timing, and stress all affect how the body processes glucose. Traditional treatment methods often used a blanket approach—standard insulin dosages and dietary advice that didn’t account for individual nuances.
That’s where AI steps in. Modern diabetes platforms now use machine learning to analyze patient-specific data from CGMs, fitness trackers, meal logs, and electronic health records. These systems learn patterns over time and offer tailored recommendations—whether it’s how much insulin to take before a certain meal, when to exercise, or how a particular food affects blood sugar.
Apps like mySugr, Glooko, and Sugarmate are integrating AI models to guide real-time decisions. Some systems can even predict how a user’s glucose will respond to future behavior—a major leap in proactive care.
Impact: AI helps personalize care in ways human clinicians simply don’t have time to do, especially at scale.
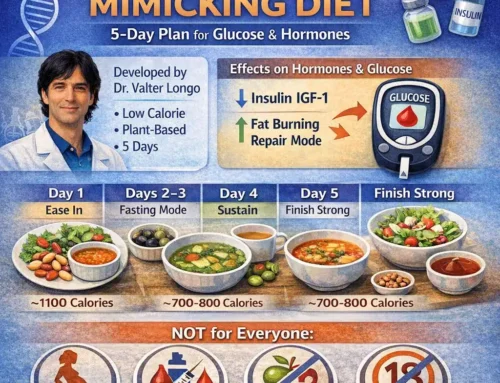
3. Predicting and Preventing Type 2 Diabetes
While managing diabetes is critical, preventing it in the first place is even more valuable. Type 2 diabetes is largely preventable with early intervention, yet millions of people slip through the cracks because traditional risk assessments rely on basic screening factors like BMI or family history.
Today, AI-driven tools are making prevention far more effective. Predictive models built from massive datasets—such as the UK Biobank or the All of Us Research Program—can identify high-risk individuals years before clinical symptoms appear. These models factor in thousands of variables: genetics, lifestyle, lab results, sleep patterns, and even socioeconomic data.
For example, researchers have developed neural network models that predict diabetes onset with over 85% accuracy. Companies like Lark and Omada Health are using AI-based digital coaching to deliver personalized prevention plans to users flagged as at risk.
Impact: Early detection leads to earlier lifestyle changes, medication, or monitoring—reducing the chance of full-blown diabetes.
4. Digital Coaching and Behavior Modification Tools
Behavior change is one of the hardest parts of managing diabetes. It’s not just about knowing what to do—it’s about staying motivated to actually do it. That’s where digital coaching platforms come in.
AI-powered apps now provide intelligent support, reminders, and feedback to help users stick to their plans. For instance, an app might recognize when a user’s glucose tends to spike after dinner and recommend walking afterwards or adjusting meal composition. Chatbot-based coaches like those in BlueStar or Lark can offer encouragement, education, and nudges in real time.
These tools work around the clock, filling in gaps between doctor visits and reducing the burden on primary care.
Impact: Digital coaching helps improve adherence to treatment plans, leading to better health outcomes without constant clinical oversight.
5. Remote Monitoring and Telehealth Integration
During the COVID-19 pandemic, telehealth exploded in popularity—and diabetes care adapted quickly. With CGMs, smart insulin pens, and Bluetooth-enabled blood glucose meters, patients can now share their health data with providers in real time from home.
AI tools help clinicians spot worrying trends faster. For instance, dashboards like Glooko’s Population Tracker use predictive analytics to flag patients with deteriorating glucose control. That allows providers to prioritize high-risk individuals for outreach or intervention.
This shift to remote monitoring is especially valuable for underserved or rural populations where regular in-person visits are impractical.
Impact: Remote tools close care gaps, catch issues early, and support continuous engagement—especially for those who otherwise fall through the cracks.
6. Accelerating Drug Discovery and Clinical Trials
AI isn’t just transforming day-to-day care—it’s also speeding up the development of new diabetes treatments.
Pharmaceutical companies are using machine learning to identify promising drug candidates faster and more efficiently. AI models can simulate how new compounds interact with human cells or predict which patient populations are most likely to benefit. Companies like Insitro and Exscientia are applying this approach to metabolic disorders, including diabetes.
Meanwhile, virtual clinical trials—enabled by wearable tech and remote monitoring—are making studies more diverse, scalable, and cost-effective.
Impact: New treatments are reaching patients faster, with more precision and lower costs.
7. Predicting and Preventing Complications
Diabetes doesn’t occur in isolation—it’s a major driver of complications like kidney disease, nerve damage, and blindness. The sooner these risks are flagged, the better.
AI algorithms are now being used to detect early signs of these complications, often before symptoms arise. For instance:
- Eye scans can be analyzed by AI to detect diabetic retinopathy with high accuracy, even in non-specialist settings.
- Predictive models can forecast which patients are most likely to develop nephropathy based on historical lab data.
- Smart insoles can monitor pressure points in the feet to predict the formation of diabetic ulcers.
Impact: Proactive monitoring and targeted intervention reduce hospitalizations, amputations, and long-term disability.
What’s Next: The Future of AI in Diabetes
Despite the progress, we’re only scratching the surface of what’s possible. Future developments may include:
- Fully closed-loop insulin delivery systems requiring zero user input.
- Non-invasive glucose monitoring through wearables like smartwatches.
- AI nutrition assistants that can analyze meals via photos and offer real-time guidance.
- Genomic AI models that tailor treatment based on an individual’s DNA.
However, challenges remain—data privacy, algorithmic bias, affordability, and digital literacy need to be addressed to ensure these tools benefit everyone, not just the tech-savvy or affluent.
Conclusion: A Smarter, Healthier Future-AI in diabetes treatment and prevention
Diabetes care is no longer confined to the clinic or pharmacy. With the power of AI and digital innovation, we now have the tools to treat more precisely, monitor more effectively, and prevent more proactively.
This isn’t science fiction—it’s already happening. But the true power of these technologies lies in their ability to humanize care. By lifting the burden of micromanagement, reducing uncertainty, and enabling earlier interventions, AI is giving people with diabetes the one thing they often lack: control.
In the fight against one of the world’s most persistent chronic conditions, that might just be the biggest game changer of all.
Related Videos:
Related Posts:
10 Revolutionary Breakthroughs Powering a Transformation in Cancer Care
Rising from the Ashes: Why I Chose to Rebuild Myself Through Advocacy
Fasting and Aging: How to Use Fasting to Boost Longevity
Resistant Starch: The Carb That Acts Like a Superpower for Your Gut and Metabolism
Be the Lighthouse, Not the Searchlight: How Real Love Finds You