Approx. read time: 8.8 min.
Post: How to Balance Female Hormones: 5 Evidence-Based Fixes
🧭 Why hormonal balance matters (and what this guide covers)
Quick note: This guide is educational, not medical care. If you have abnormal bleeding, severe pain, missed periods, or new symptoms, talk to your clinician promptly.
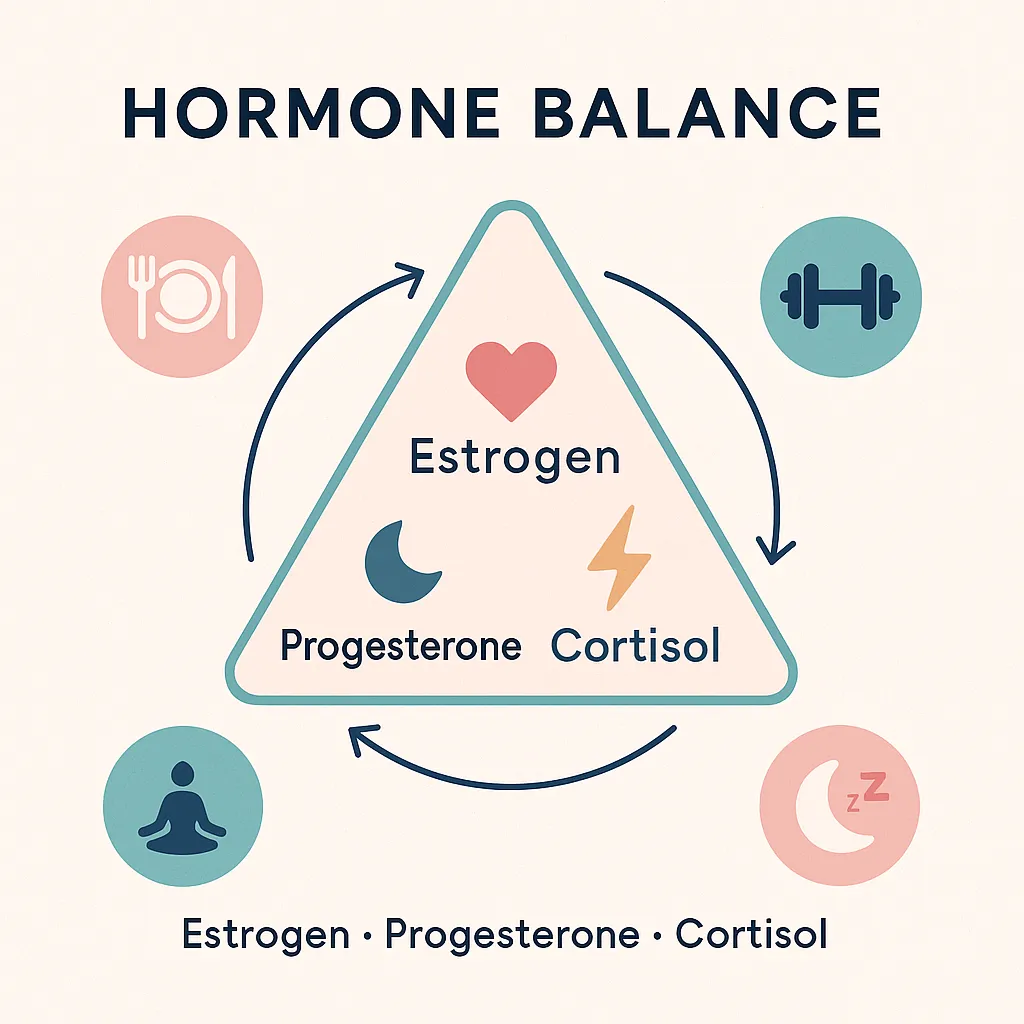
Estrogen, progesterone, and cortisol shape mood, metabolism, sleep, cycles, skin, bones, and energy. When they drift out of rhythm, you may feel it as anxiety, fatigue, brain fog, weight gain, hot flashes, or irregular periods. The good news: everyday habits—eating patterns, sleep, movement, and stress skills—can nudge hormones back toward balance. Below you’ll get:
-
Plain-English basics of the “big three” hormones
-
A five-pillar plan that works at any age
-
Life-stage playbooks (20s, 30s–early 40s, perimenopause, menopause)
-
Evidence-informed supplements (with cautions)
-
A realistic sample day, lab pointers, and FAQs
🧬 Meet the Big Three Hormones
💖 Estrogen (structure, mood, bones)
Estrogen supports the uterine lining, brain, skin, and bone density; it rises in the follicular phase and peaks around ovulation. When estrogen dips in midlife, hot flashes and sleep disruption can appear; later, bone health needs extra support. Guidance from The Menopause Society recognizes hormone therapy as the most effective treatment for vasomotor symptoms when appropriate.
🌙 Progesterone (calm, sleep, cycle stability)
Progesterone is dominant after ovulation (luteal phase). It steadies mood, eases anxiety for many, and supports deep sleep. Low progesterone can amplify PMS-type symptoms and make cycles feel “louder.”
⚡ Cortisol (the stress metronome)
Cortisol helps you wake, mobilize fuel, and respond to stress. Chronic elevation can sap progesterone, worsen sleep, and increase abdominal weight. Mindfulness and breathwork practices show measurable reductions in cortisol in randomized trials and meta-analyses.
🍽️ Core Pillar 1 — Balance blood sugar to steady hormones
Glucose spikes tug on cortisol and can worsen PMS, cravings, and energy crashes. Practical, evidence-informed ways to smooth the curve:
-
Build meals around protein + fiber + healthy fats. Protein and fat blunt post-meal glucose compared with carb-heavy meals.
-
Prefer lower-GI carbs and intact whole grains; fiber slows absorption and reduces glycemic response.
-
Try a 10-minute walk right after meals—shown to lower post-meal glucose in adults.
🧪 Core Pillar 2 — Support natural detox & elimination (liver + gut)
Your liver chemically modifies “used” estrogens; your gut helps excrete them. You don’t need extreme cleanses—just consistent habits:
-
Eat cruciferous vegetables (broccoli, kale, cabbage) often; they’re rich in compounds that influence estrogen metabolism. (Supplements like DIM exist; see supplement section for cautions.)
-
Hit 25–35 g fiber/day (vegetables, legumes, oats, chia) to keep things moving—fiber lowers glycemic response and supports elimination.
-
Hydrate and limit alcohol; alcohol can aggravate sleep and hot flashes and adds liver workload.
🦠 Core Pillar 3 — Care for your gut
A healthy microbiome (including the estrobolome) helps process hormones. Practical basics: diverse plants, fermented foods (yogurt, kefir, kimchi), and consistent fiber. If you have ongoing GI symptoms, get them checked—gut issues and hormone symptoms often travel together.
😴 Core Pillar 4 — Sleep like it’s your superpower
Adults do best with 7–9 hours most nights; less than 7 is linked to metabolic and mood issues. Treat sleep like a keystone habit: consistent bed/wake times, cool/dark room, light exposure in the morning, and gentle wind-down at night.
🧘 Core Pillar 5 — Train your stress response
Chronic stress pushes cortisol up and nudges sex hormones off-beat. Science-backed stress skills:
-
Mindfulness & meditation (10–15 minutes) reduce cortisol in controlled trials.
-
Slow breathing (e.g., 4-6 breaths/min) improves stress markers and mood.
-
Light daily movement and nature walks complement the effect (and help blood sugar).
🧯 Reduce endocrine disruptor load (small swaps, big win)
Some chemicals (e.g., BPA) can act like hormones. Lower exposure with simple swaps: use glass/stainless for hot foods, avoid heating plastic, and go fragrance-free where possible. See credible overviews from NIEHS and CDC.
🗓️ Your 20s — Build a resilient rhythm
Common: irregular cycles, PMS, acne, stress-related flares
Do now:
-
Track cycles (app or paper).
-
Lift or body-weight train 2–3x/week and walk daily.
-
Eat protein at breakfast; pair carbs with fiber/fat.
-
Curious about “seed cycling”? It’s popular, but human evidence is limited; enjoy seeds for their nutrition without banking on cycle-specific effects.
👩💼 Your 30s & early 40s — Protect ovulation & progesterone
Common: Estrogen dominant symptoms, PMS, fatigue, low libido
Focus: steady glucose, stress care, micronutrients for ovulation (protein, zinc, B vitamins), and strength training.
-
Consider Vitex (chasteberry) for PMS—meta-analyses suggest benefit, though trial quality varies; discuss dosing/timing with your clinician.
-
Keep annual labs current; address iron, thyroid, and vitamin D as needed (with your provider).
🔄 Perimenopause (mid-40s to early-50s) — Ride the fluctuations
Common: hot flashes, night sweats, anxiety, brain fog, irregular cycles
Strategies:
-
Prioritize sleep and stress downshifts (breathwork, mindfulness, lighter evening meals).
-
Choose lower-impact cardio + resistance work; intensity is fine if recovery is solid.
-
Nonhormone options exist; evidence summaries from The Menopause Society can help you discuss choices with your clinician.
🌙 Menopause (50s+) — Sleep, strength, and bones
Estrogen and progesterone are lower; bone and sleep need extra attention.
-
Resistance training (and mixed aerobic + resistance) supports bone mineral density in postmenopausal women. Aim for 2–3 sessions/week.
-
Hormone therapy (HRT/MHT) is the most effective treatment for hot flashes when appropriate; discuss risks/benefits and timing with your clinician (often most favorable within 10 years of menopause onset).
-
Food first; some find soy foods modestly reduce hot flashes (results are mixed).
💊 Evidence-informed supplement guide (use with clinician)
| Goal | Supplement | How it may help | Notes & evidence |
|---|---|---|---|
| Lower perceived stress / cortisol | L-theanine, breathwork practice | Calming effect; breathwork reduces stress markers | Mindfulness & related practices can reduce cortisol in RCTs; pair with sleep care. |
| PMS symptom relief | Vitex (chasteberry) | May improve overall PMS scores | Meta-analyses show benefit with cautions about bias/heterogeneity; discuss dosage & interactions. |
| Support estrogen metabolism | DIM (from crucifers) | Shifts estrogen metabolites in some studies | Human clinical data are limited; consult before use. Food sources are safe for most. |
| Support estrogen elimination | Calcium-D-glucarate | Inhibits beta-glucuronidase (animal & mechanistic data) | Human trials for hormone balance are lacking; discuss risks/benefits. |
| Cycle regulation / insulin sensitivity (esp. PCOS) | Myo-inositol | Often used for ovulatory support and insulin signaling | Review with a clinician; check for interactions and appropriate dosing. (Evidence base evolving.) |
| Sleep and mood support | Magnesium glycinate | Commonly used for sleep quality and PMS | Match form to tolerance; align with dietary intake; monitor if on meds. |
| Hot flash relief (modest) | Soy isoflavones (from food first) | Small average reductions in hot flash frequency/severity | Results are mixed; foods preferred; discuss if you have a hormone-sensitive cancer history. |
Always review supplements with your healthcare provider—especially if you’re pregnant, trying to conceive, have thyroid/breast conditions, or take prescription meds.
🗺️ Sample day (perimenopause: estrogen-dominant + high-cortisol profile)
Morning (light anchor):
-
Wake at a consistent time; get daylight in your eyes.
-
Breakfast: eggs + sautéed greens + avocado; or Greek yogurt + chia + berries.
-
10-minute outdoor walk after eating.
Midday (steady energy):
-
Lunch: salmon bowl (quinoa, cabbage slaw, edamame, sesame).
-
3–5 minutes of slow breathing before returning to work.
Afternoon (protect sleep):
-
Herbal tea; skip caffeine after ~2 p.m.
-
Protein snack (cottage cheese + fruit; or hummus + veg).
Evening (cool down):
-
Dinner: chickpea curry with broccoli + brown rice.
-
15 minutes of gentle yoga, legs-up-the-wall, or a warm bath.
-
Devices down 60 minutes before bed; lights low.
-
Aim for 7–9 hours of sleep.
🧩 Smart labs & check-ins (talk with your clinician)
-
Cycle timing matters. If testing sex hormones, ask about follicular vs. luteal timing.
-
Discuss: CBC/iron studies, TSH, vitamin D, lipid panel, A1C (especially if you’ve had gestational diabetes or insulin resistance).
-
In midlife, talk through HRT/MHT options; ACOG’s patient guide is a solid primer before your visit.
❓ FAQs
Q1. What’s the fastest way to start balancing hormones?
A. Pick one lever you’ll actually do daily: protein-forward meals, a 10-minute post-meal walk, or a 10-minute wind-down before bed. Even small steps improve glucose control, stress, and sleep—key inputs to hormone health.
Q2. Is seed cycling necessary?
A. No. Seeds are nutritious, but cycle-timed seed protocols lack strong human evidence. Enjoy flax, pumpkin, sesame, and sunflower anytime.
Q3. Can I balance hormones without cutting all carbs?
A. Yes. Focus on carb quality (lower-GI, higher-fiber) and pair carbs with protein/fat.
Q4. Do I need hormone testing to start?
A. Not to begin lifestyle steps. Testing can be helpful for persistent symptoms, missed periods, fertility goals, or midlife treatment decisions—coordinate with your clinician.
Q5. Is HRT safe?
A. For many healthy women near menopause, benefits outweigh risks for hot flashes and sleep problems. It’s individualized; read The Menopause Society overview and talk to your clinician.
Q6. What about DIM and calcium-D-glucarate?
A. DIM can shift estrogen metabolites; calcium-D-glucarate affects elimination in animal/mechanistic data. Human evidence is limited—use with clinician guidance.
Q7. Which exercise is best in menopause?
A. A mix: resistance training for bones/muscle, plus moderate cardio and daily walking.
Q8. Can soy help hot flashes?
A. Soy foods may modestly reduce hot flashes for some; results are mixed. Food first over pills.
Q9. How much sleep do I actually need?
A. Most adults do best with 7–9 hours. Less than 7 is linked to worse metabolic and mood outcomes.
Q10. Are plastics really a problem?
A. BPA and some plasticizers can act like hormones. Using glass/stainless and avoiding heating plastics reduces exposure.
Q11. Will a 10-minute walk after dinner do anything?
A. Yes—post-meal walks can lower the glucose spike meaningfully.
Q12. I’m not “perfect” with habits. Is it still worth it?
A. Absolutely. Hormones respond to trends, not one day. Small wins, repeated, beat intense sprints.
✅ Your “how to balance female hormones” checklist
-
Protein + fiber + healthy fats each meal; lower-GI carbs.
-
Walk 10 minutes after meals.
-
Breathwork or mindfulness most days.
-
Sleep 7–9 hours; protect your wind-down.
-
Strength train 2–3x/week (add gentle cardio).
-
Reduce endocrine disruptors (glass over plastic, fragrance-free).
-
Use supplements thoughtfully with your clinician.
Final thoughts
Hormonal imbalance rarely arrives overnight—and it rarely resolves overnight. But your body is adaptable. Build meals that calm blood sugar, defend your sleep at all costs, move most days (especially lifting and short post-meal walks), and practice one simple stress skill. Layer in food-first phytonutrients, and discuss HRT or targeted supplements with your clinician when appropriate.
Related Videos:
Related Posts:
AI for Workplace Burnout 25 Practical Ways to Fix Work Without Breaking
Protect Your Mood Around Toxic People 12 Proven Moves
Protect Your Health from Stress 16 Proven Relationship Tactics
AI in PTSD Therapy 8 Game Changers for Care
Explosive Insights on AI Mental Health Apps 15 Pros, Cons & Real-World Tips